Home » Glaucoma
Glaucoma
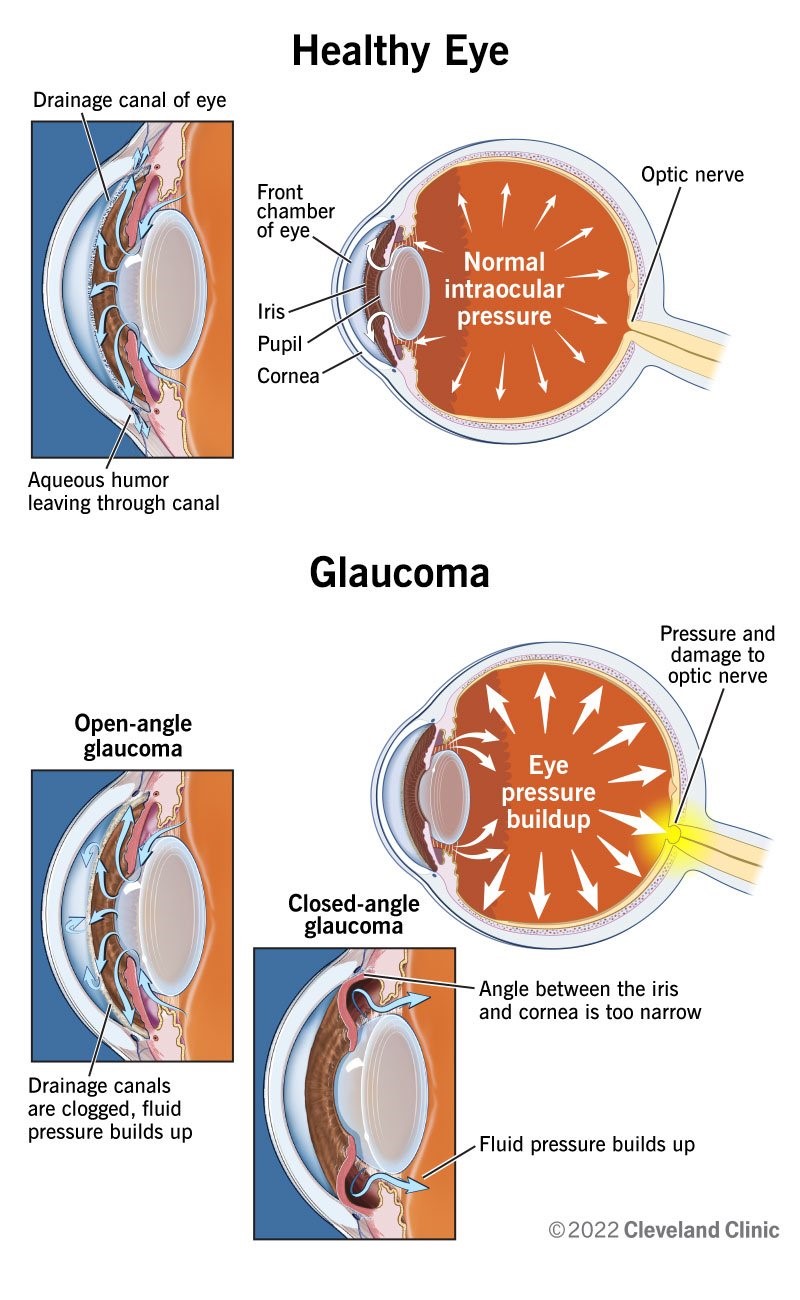
Glaucoma is a leading cause of blindness worldwide. It is a condition which affects the back of the eye, specifically the optic nerve – the cable that connects the eye to the brain. The damage to the nerve results in progressive loss of vision, generally starting with side vision and eventually eating away at central vision.
There are many types of glaucoma – the most common is called open angle glaucoma, followed by narrow angle glaucoma. While we do not completely understand why the damage occurs at the optic nerve, we know high pressure inside the eye is the most identifiable factor. There is no cure for glaucoma. Currently the only management for glaucoma is lowering eye pressure.It is important to understand once vision loss occurs, it cannot be regained, thus treatment is crucial to slow or prevent disease progression. Treatment will likely be for the rest of your life
What are the risk factors?
Older age, family history, smoking, diabetes, hypertension, certain medications, thin corneas to name a few. There is also a higher incidence in Black, Hispanic and Asian backgrounds.
How is glaucoma diagnosed?
We carefully screen for signs of glaucoma in all our visits by measuring the pressure in your eyes, looking at the back of your eyes to evaluate the health of the optic nerves, and running appropriate tests as needed such as visual fields and scans of the nerves.
What are the symptoms?
With open angle glaucoma, there are generally no symptoms until later stages of the disease when the visual field (side or peripheral vision) becomes progressively smaller, until central vision is eventually affected.
Closed and narrow angle
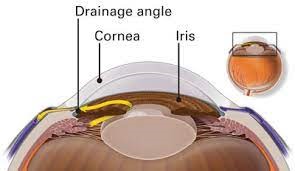
The angle of the eye is the meeting place of the cornea, the clear front part of the eye, and the iris, the colored part of the eye. This area contains the mechanism that controls the pressure of the eye called the trabecular meshwork. Our eyes contain a fluid, which is different from our tears, which is drained through this angle – similar to a drain in a sink. In some people, the angle is narrow.
It is important to understand that just by having narrow angles does not mean you have or will have glaucoma. However if the fluid is not draining properly, or if this angle suddenly closes, the pressure in the eye can become dangerously high, and glaucomatous damage may occur.
Depending on the structure, your eye care professional may recommend a laser procedure either LPI (laser peripheral iridotomy), or iridoplasty, to help open up this angle and prevent angle closure attacks.
LPI (Laser peripheral iridotomy)
A laser procedure which is performed in office to create an additional area for fluid to drain out of, and help open up the angle. It is fast and virtually painless. No special measures need to be taken by the patient – patient is able to go about usual activities before and after procedure. Usually if one eye requires this procedure, your other eye will as well. However, you will have to come back to have the other eye done on a separate visit – we do not perform this procedure on both eyes on the same day.
In cases where the angle is extremely narrow, or the laser was not effective, you may require a lensectomy, which involves removing the eye’s natural lens (as in cataract surgery) to further open the angle.
** Patients with narrow angles should be aware of the signs and symptoms of angle closure attack — characterized by intense eye pain, halos around lights, redness, vomiting and blurred vision. If this occurs it is an emergency and you must present to your eye doctor right away to stop irreversible damage.
Pseudoexfoliation
A condition involving dandruff like material that build up in different parts of the body including in the eye. The material builds up and blocks the trabecular meshwork – the area that regulates the pressure inside the eye. Pseudoexfoliation often results in a very aggressive form of glaucoma, causing more rapid vision loss and often blindness. For this reason, patients with Pseudoexfoliation require more aggressive treatment.
More on eye pressure…
Patients often ask what is a “normal” eye pressure – this is a difficult question to answer because truthfully “normal” is different for everyone. In general, for a non-glaucomatous eye, normal pressure can range from 10-21. However, in some eyes a pressure of 25 may be normal and not cause problems, while in other eyes a pressure of 11 may be too high.
In patients with glaucoma, stage of the disease, corneal thickness, progression, family history and response to treatment are all considered when deciding what a good pressure is.
Managing eye pressure
Treatment revolves around lowering and maintaining eye pressure
Eye drops –the most common treatment and involves instilling pressure lowering drops into the eye generally from one to four times daily. There are many different kinds of drops and patients may be put on multiple drops to control pressure. It is essential to use the drops daily as directed. Some drops require refrigeration.
Laser – there are various types of in-office laser treatments that take approximately 6 weeks to start taking affect and may be repeated as needed
Injectable medication — an in-office procedure in which a small device is implanted into the front of the eye and slowly releases medication
Surgery – in advanced cases when conservative management does not achieve the desired pressure lowering effect, surgery is required.